Written by Dr. Clarence Temple
Paris Texas in 1969 was a many-faceted city. In addition to being the county seat of Lamar County, it was also the retail hub for a large part of northeast Texas and southeast Oklahoma. It was known as an important medical center with a reputation for having outstanding primary care and specialty physicians. Paris also had two new 150 bed hospitals: St. Joseph’s Hospital, located just east of downtown, and McCuistion Medical Center on North Loop 286.
The city had for years been home to prominent state political figures, led by Senator A.M. Aiken, longtime chairman of the Senate Finance Committee.
Paris had many industries, including Babcock and Wilcox, Uarco Printing, Philips Lighting, National Hardware and others. It was also the site of Campbell Soup’s newest plant.
Education in Paris was led by Paris Junior College recognized as an outstanding two-year institution. School systems included Paris ISD, North Lamar, Prairiland, Delmar, West Lamar, and Roxton ISD’s.
Water supply is critical to the success of any community. Pat Mayes Reservoir was just completed and provided outstanding recreational facilities for the region as well as a secure water source.
While the medical community was composed of excellent physicians throughout the city, the doctors by and large confined their practice to one hospital or the other, but rarely both. The physician’s office was usually located near the hospital in which he or she practiced. This rift extended to some degree to the city as a whole with some people saying, “We go to St. Joseph’s” and others saying, “We use McCuistion”.
St. Joseph’s hospital was owned and administered by the Sisters of Charity, a Catholic organization. McCuistion Medical Center was owned and operated by L.P. McCuistion Foundation for whom the hospital was named after.
Competition between the two hospitals, each opening in 1968 and each replacing outmoded facilities, was strong, but maintained at a highly respected level. The Lamar-Delta County Medical Society met monthly and was well attended by members of both hospital staffs. At this meeting, members of the two staffs melded into one organization if only for that evening.
Both hospitals had increasingly busy emergency rooms with coverage provided by members of their medical staffs. Neither hospital had emergency physicians or hospitalists, and the admitting physician made rounds on his or her patients once or twice daily.
With excellent physicians on each staff providing coverage in primary care, internal medicine, general surgery, obstetrics and gynecology, pediatrics, ophthalmology, otolaryngology, radiology, pathology, and doing so in the new state of the art hospitals, people in Paris and surrounding cities were provided with a level of medical care typically found only in cities two or three times the size of Paris.
Although Paris at that time had no trained orthopaedic surgeon, routine fracture care was provided by family physicians and general surgeons in the community. If more advanced care was required it was usually provided by Dr. Bernard McConnell of Greenville, Texas. Dr. McConnell was a superb orthopaedist who would travel to hospitals in the area surrounding Greenville, including Clarksville, Mt. Pleasant, Sulphur Springs and other towns. He also maintained a very busy practice in Greenville. He was held in high regard by patients and physicians alike.
In 1969, orthopaedic surgeons were usually found only in larger cities in Texas outside of metropolitan areas in the state (populations of fifty thousand or more). Only Greenville, Lufkin, Nacogdoches, Kerrville, and possibly one or two other cities had an orthopaedist in residence. Paris joined that group in 1969.
Dr. Clarence Temple, a native of Mt. Pleasant completed his residency in orthopaedic surgery at Vanderbilt University Hospital in Nashville in June 1969. He and his wife Carolyn with their four sons moved to Paris in order to be back in northeast Texas and to live in a smaller city. While his office was located adjacent to McCuistion, he wanted to be a Paris orthopaedist and to work in both hospitals. He was accepted to the staff of both St. Joseph’s and McCuistion. His office opened July 11, 1969. Dr. Clarence Temple provided excellent orthopedic care to his patients for thirty-six years and retired from Paris Orthopedic Clinic on December 31, 2005.
The practice grew rapidly drawing patients from surrounding communities in Texas and Oklahoma. Both Paris hospitals were very supportive in developing the new practice.
The reputations of the Paris hospitals and the excellent physicians on their staffs were primary factors in the successful beginning of what was to become Paris Orthopedic Clinic.
In 1974, Dr. Frank Wood and Michael Milek joined Dr. Temple. They were graduates of the Vanderbilt program. The three orthopaedists having outgrown the initial clinic facility, moved into a new clinic building at 785 Lewis Lane. This building not only provided much needed examination and office space, but included expanded radiology facilities and later physical therapy under the leadership of Douglas Wehrman, LPT.
After three years, Dr. Milek returned to Vanderbilt to direct the hand surgery program. Dr. Gary Forster joined Drs. Wood and Temple. Dr. Forster, a native Californian, completed his orthopaedic training at Baylor College of Medicine in Houston.
The practice continued to grow and Dr. Mark Nardone, a native of Pennsylvania and a graduate of Bowman Gray University orthopaedic program joined POC. His strong backing of the Philadelphia Eagles led to some interesting non-medical discussion. Dr. Nardone left POC on February 29, 2004
Dr. Forster then decided to return to the west coast, moving to the state of Washington. Dr. Robert Schneider, a native of Illinois who did his orthopaedic training at the University of Texas Southwestern Medical School in Dallas, joined POC. His first year in practice was named by his being a primary provider in the superb response of our medical community to the disaster of the Paris tornado on April 2, 1982. Dr. Schneider was part of the face of Paris medicine in his interviews on Dallas television channels. Dr. Schneider left POC on December 31, 2009.
The increasing need for orthopaedic care in our part of the state led to the opening of a second office. This located on the St. Joseph’s campus. Dr. Wood and Schneider were in practice at the new location while Drs. Nardone and Temple remained at the Lewis Lane location.
Dr. Steven Rowlan is a native Oklahoman. He grew up in Oklahoma City, graduated from the University of Oklahoma, the OU Medical School and completed his orthopaedic residency at University Hospital. He joined POC in 1983. Like each doctor who has joined POC, Dr. Rowlan made an immediate and lasting contribution to the improvement of services and to the character of this clinic.
Dr. Jeffrey Neilson, also an Oklahoman, did his residency in orthopaedics at Scott & White Clinic in Temple. He joined POC in 1989. Dr. Neilson was the primary orthopaedist in developing the POC Clinic in Sulphur Springs. Dr. Neilson left POC on December 31, 2011.
Dr. Thomas Carrell joined POC in 1990. He also completed his orthopaedic training at Scott & White in Temple. Dr. Carrell is a strong advocate of personal physical fitness and he has participated in triathlon activities. Dr. Carrell left POC on September, 10, 2007.
At this point, the offices at St. Joseph and at Lewis Lane were becoming crowded. A new clinic was planned and construction at the present location at 3435 Northeast Loop 286 was begun. The new POC building was constructed by Harrison Walker and Harper and was finished in 1993. The new clinic allowed all the orthopaedists to office in one location exactly halfway between the two hospitals. It also provided the presence of at least one orthopaedist in each hospital at any time during the day.
In 1992, Dr. Drew Temple joined Paris Orthopedic Clinic. He is a graduate of Texas A&M, Texas A&M School of Medicine, and did his residency at University of Arkansas. He has provided a stimulus to continued improvement which is reflected in the entire clinic. He also has a secondary specialty in sports medicine.
Dr. David De la Garza joined POC in 2001. Dr. De la Garza is a graduate of Texas A&M and completed his residency at Texas Tech School of Medicine. He has been the source of many original approaches to challenging cases.
In 2003, Dr. Greg Green joined POC having completed his residency at Duke. A native of Colorado and graduate of Stanford and Baylor School of Medicine, Dr. Green is a strong addition to the Paris medical community.
Dr. Mark Gibbs is a native Parisian. He is a graduate of University of Texas Medical Branch and completed his residency at the University of Tennessee Campbell Clinic. He joined POC in 2011 and has a secondary specialty of sports medicine.
Dr. Michael Elliott is a native of Arizona. He is a graduate of University of North Texas Health Sciences Center –Texas College of Osteopathic Medicine and completed his residency at John Peter Smith Hospital in Fort Worth. He has an orthopedic subspecialty in sports medicine. He joined POC in 2014.
Leah Baldwin, PA-C joined POC in 2011. Leah is a graduate of University of Wisconsin Physician Assistant Program. Leah was a Second Lieutenant in the Wisconsin Army National Guard prior to joining Paris Orthopedic Clinic.
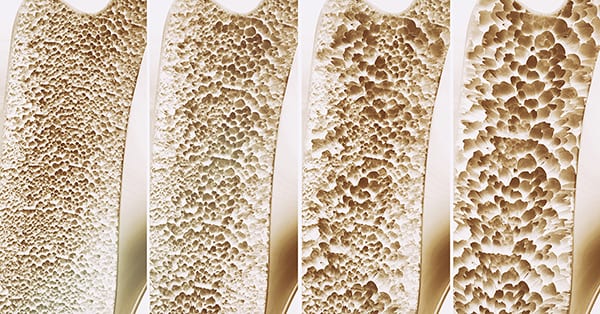
Carmen Holmes, PA-C joined the POC team in 2014. She is a Paris native and graduate of University of Texas Southwestern Medical Center Physician Assistant Program. While practicing general orthopedics, she also has a special focus on osteoporosis treatment.
With the addition of sports medicine subspecialties, Paris Orthopedic Clinic’s name was changed to Paris Orthopedics and Sports Medicine in 2016.
Paris Orthopedic Clinic has been fortunate in having strong leadership in its business managers. Bill Mercy was the first and was followed by David Eisele. Michael Miller is now the POC business manager.
The employees of Paris Orthopedic Clinic are the foundation of the smooth day-to-day functioning of the clinic. The supportive care given by them to each patient is an important factor in their treatment. In addition to providing orthopedic care to a large part of northeast Texas and southeast Oklahoma for the past fifty years, physician members of the clinic have provided leadership in our hospitals and city. POC has been prominent in the Texas Orthopaedic Association and in the American Academy of Orthopaedic Surgery, and two members of POC have served as examiners for Part II of the ABOS Boards.
Paris Orthopedic Clinic has been recognized as a one of the premier general orthopaedic surgery clinics in the state of Texas. Its physicians and staff look forward to the next fifty years.